HIV rates have been on the decline in the U.S. for years now, but stark disparities remain, with some groups of people at high risk of infection.
Here's the good part: The number of people diagnosed annually has dropped by about 20 percent in the last decade.
The drop was driven by plunges in certain groups of people, including heterosexuals, with a 35 percent decline since 2005; black women, with a 42 percent decline; and people who inject drugs, 63 percent.
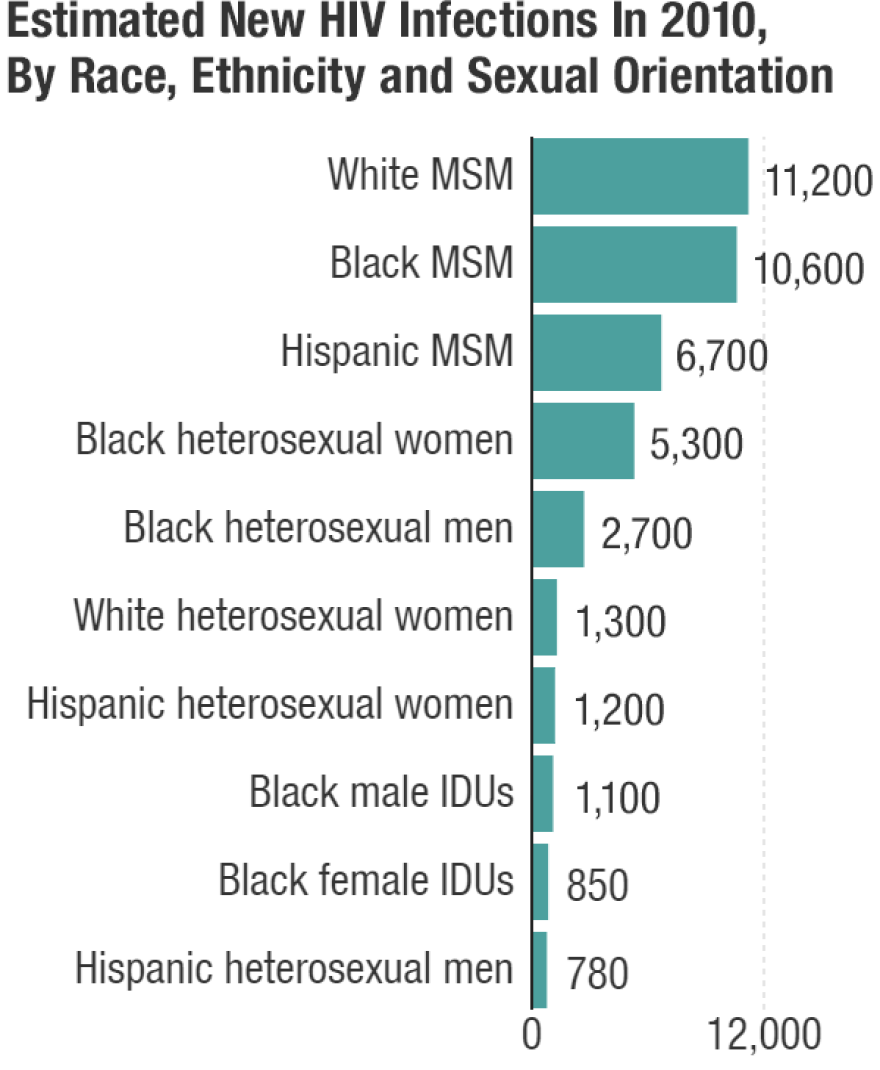
But that leaves this bad part: Rates are increasing in African-American and Hispanic men who have sex with men, according to data released Tuesday by the Centers for Disease Control and Prevention. At current rates, half of black and one quarter of Latino gay or bisexual men will be diagnosed with HIV in their lifetimes.
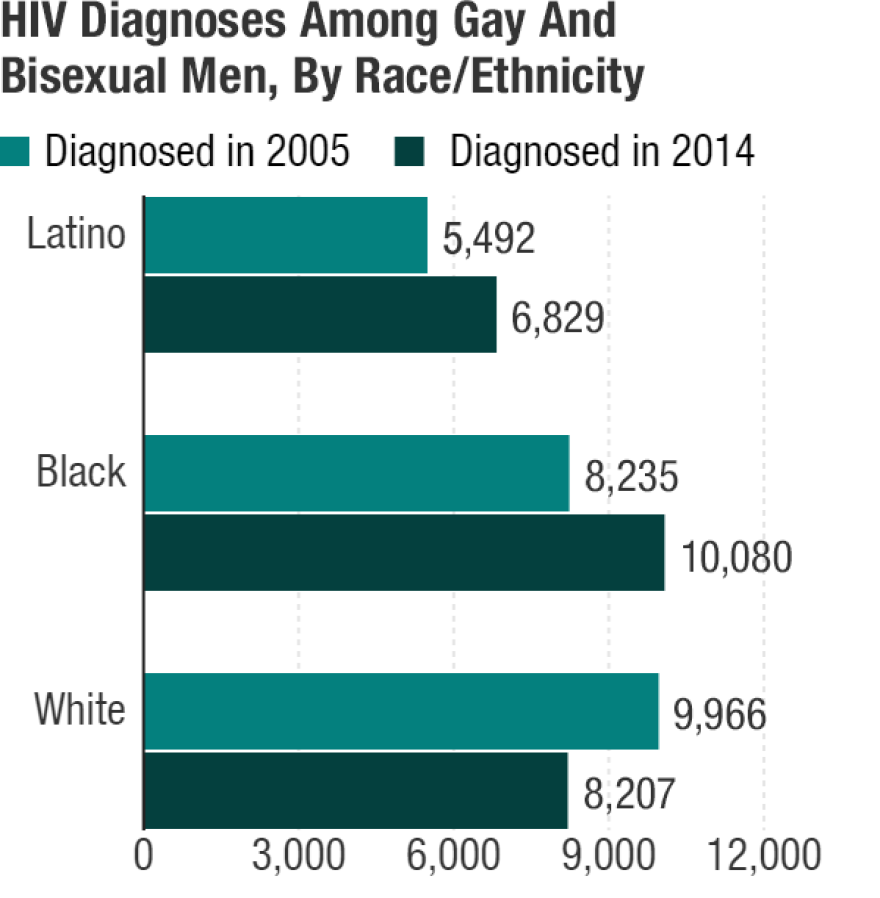
In the last 10 years, diagnoses increased about 6 percent among all men who have sex with men, but rose 22 percent in black men and 24 percent in Latino men.
There were concerning increases over the decade among Asian American and American Indian/Alaska Native men who have sex with men, too, but the absolute numbers are tiny compared to those of other racial groups.
Men who have sex with men account for about 2 percent of the U.S. population, but almost 70 percent of the country's HIV diagnoses.
To find out why these numbers are so high, Shots talked to Juan Carlos Loubriel, director of community health and wellness at Whitman-Walker Health in Washington, D.C., where one in 13 people will be diagnosed with HIV over the course of their lifetime. He's originally from San Juan, Puerto Rico. The conversation has been edited for length and clarity.
When you were just entering the field of HIV prevention and care, you found out that your dad had it.
Actually it was not HIV, it was AIDS. By the time I knew he had AIDS, he was not conscious anymore.
He'd known he had HIV and he kept it a secret?
Yeah, he knew he had HIV and he knew I was working in the field with HIV ... I knew as a fact that he was a bisexual man, but we never talked about it. You know as Latinos, you don't talk about that kind of stuff. I'm gay myself and I never talked to him about it. It would have been very nice to talk about both feelings.
I didn't know that he knew [about his HIV diagnosis] until I was cleaning his apartment and I found HIV test results from five years before. So he knew a long time ago and never talked about it. And he never sought treatment. Even though the treatment was not the best treatment on the market, he could have probably been alive right now.
Why didn't he seek treatment?
We have improved a lot since HIV was called the "gay cancer," but some of the stigma is still in the community — stigma about being gay, stigma about being bisexual, stigma about a Latino bisexual man telling a provider that he was having sexual encounters with another man. That would have been terrible for him, I'm sure. So, the machismo plays a big role in the community and [so does] lack of knowledge about HIV.
What leaped out at me in this new data is that there's been progress in reducing the number of new HIV cases overall, but not among Latino and black men who have sex with men (MSM).
Yeah, it's shocking, right? This mirrors basically what we are seeing here in the city. And this is slightly overall progress, so we need to see that. But also we need to see that if we don't have a wake-up call and we don't act and we are not addressing those social determinants that are affecting our community, things will go as the CDC said, and the MSM will [have] one of the highest rates ever.
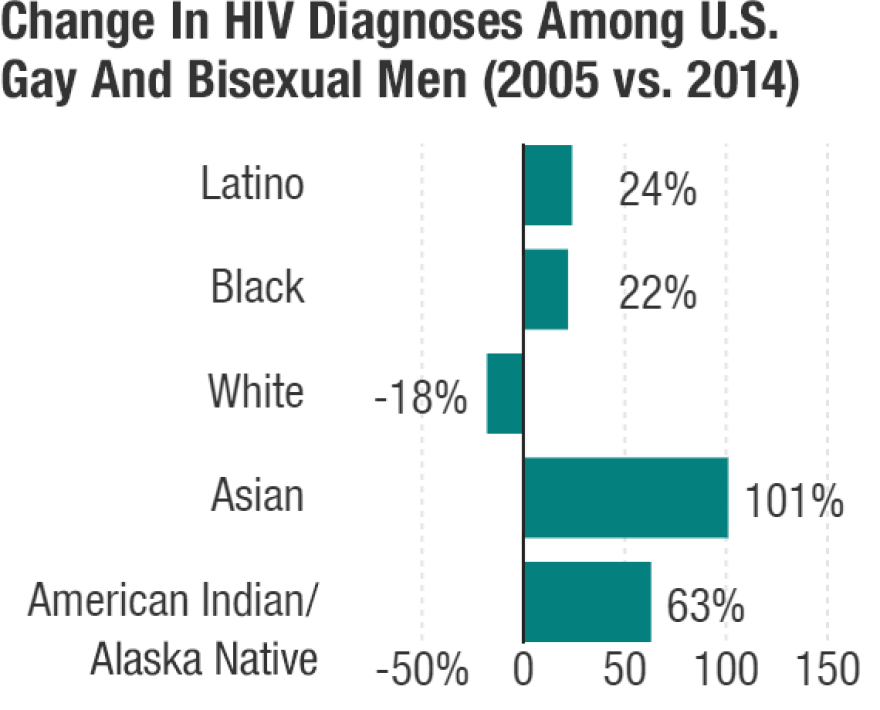
White men who have sex with men actually saw an 18 percent decline in diagnoses in the last decade. What are African-American and Latino men up against that's increasing their risk?
It's a continuation of the cultural factors that affect HIV infection. So Latinos that avoid seeking testing, they avoid the health care system because of stigma, because of the immigration status, because if they are MSM, the machismo in the community plays a big role. There's a huge, huge, huge, huge stigma around homosexuality in the Latino community. Also, you can look at the socioeconomic factors that are kind of like [those among] African Americans – the immigration patterns, lower education, limited access to health care, all those factors that also affect the population — our population. And you know, Latinos have the third highest incidence of sexually transmitted infections (STIs), so that means that makes them more vulnerable to get HIV.
Because they're already sick with something else?
Correct. Because if you have one STI, that makes you more likely to get HIV. That's a fact.
Since the first AIDS diagnoses in the U.S. were made 30 years ago, the white MSM community has worked hard to build awareness and resources for preventing and treating HIV. Are the same resources available to these other groups we're talking about? Do they need to have separate movements?
We are still trying to figure it out — all of us who work in public health — because it has been very difficult. It's a combination of multiple factors that makes a population more vulnerable to get HIV.
Stigma and discrimination prevent the Latino community from seeking high quality health care services. And this is where we are trying to go back and utilize those methods that have worked – like peer-to-peer education. In another community you can disseminate information and everyone gets it.
So, you're saying public health outreach attempts don't make it to all these populations equally?
Correct.
What are some other gaps in getting prevention and care to the African-American and Hispanic communities?
Access to health care. That is very important. That is one of the first ones.
We need to continue the education and we need to bring [to these communities] what worked well. We know as a fact what worked well is funding access for HIV testing. We know as a fact it worked well to detect HIV at an early stage, to use treatment as a prevention, and reducing the viral load of a community. We have new tools that we need to utilize. It's up to us to push it. We have now PrEP [ Pre-exposure prophylaxis to prevent infection], but it has been a pattern that among African Americans and Latinos, they don't know yet what PrEP is.
We have the tools to stop HIV; we have the tools to change these data definitely. And we need to work more with all the complex factors that I have talked about and also pushing what worked well.
You know, PrEP was not here five years ago. I think people don't realize — like with my dad who passed away because he had AIDS — if that pill was available back in the day, he wouldn't have had HIV.
The CDC estimates about 1.2 million people are living with HIV in the U.S. and about 40,000 people are diagnosed each year. Any other numbers you think people should know about?
Lifetime risk of HIV diagnosis in different groups. MSM: 1 in 6. Women who inject drugs: 1 in 23. Men who inject drugs: 1 in 36. African American MSM: 1 in 2. Hispanic MSM: 1 in 4.
These numbers are real, and if we don't wake up and we don't act now, we will see these numbers go higher.
Copyright 2020 NPR. To see more, visit https://www.npr.org. 9(MDAxMzY2MjQ0MDEyMzcyMDQ5MzBhZWU5NA001))



